What is the Endometrium?
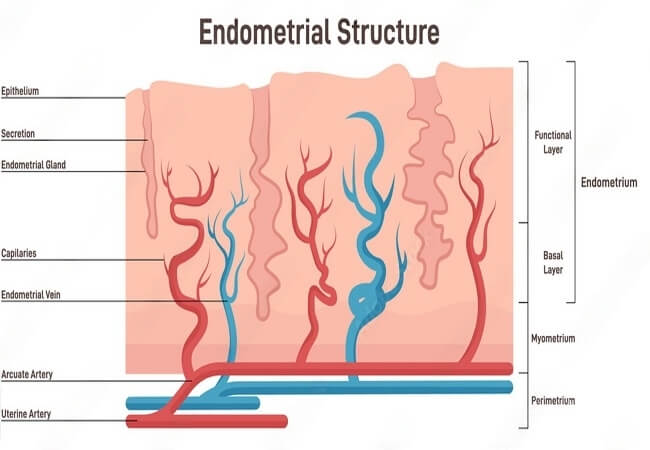
The endometrium is the inner lining of the uterus, a vital part of the female reproductive system. It undergoes remarkable changes throughout the menstrual cycle, preparing the uterus for a potential pregnancy. Comprised of two layers, the functional and basalis, the endometrium serves several critical functions:
- Menstruation: If fertilization doesn’t occur, the functional layer sheds during menstruation, expelling blood and tissue through the cervix and vagina.
- Implantation: The endometrium thickens in preparation for implantation, allowing a fertilized egg to attach and develop into an embryo.
- Nourishment: The endometrium supplies nutrients to the developing embryo, ensuring its proper growth.
What is Endometrial Hyperplasia?
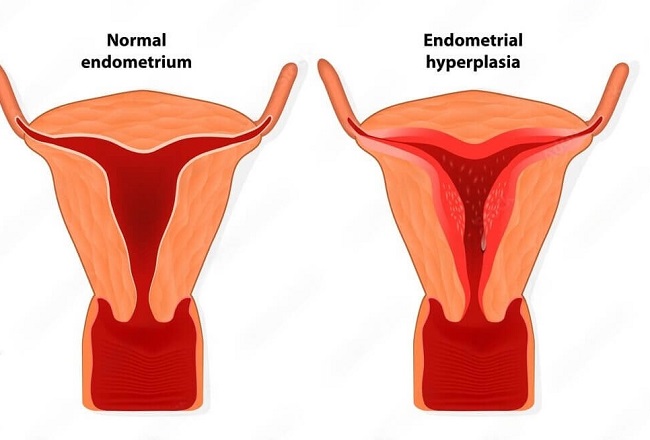
endometrial hyperplasia
Endometrial hyperplasia is a condition characterized by the abnormal thickening of the endometrial lining. The primary cause is an imbalance of the hormones estrogen and progesterone, which regulate the endometrium’s growth and shedding. Endometrial hyperplasia has four types:
- Simple Hyperplasia: Enlargement of the endometrium without abnormal cell growth.
- Complex Hyperplasia: Overgrowth of endometrial glands, creating a denser appearance.
- Simple Atypical Hyperplasia: Enlargement with abnormal cell growth, but no precancerous changes.
- Complex Atypical Hyperplasia: Overgrowth of endometrial glands and abnormal cell growth, posing a higher risk for endometrial cancer.
Normal Endometrial Thickness:
endometrial thickness
The range of endometrial thickness, and specific sizes like 14 mm or 1.5 cm. The endometrium is the inner lining of the uterus that undergoes changes during a woman’s menstrual cycle. Its thickness varies depending on the phase of the cycle. The endometrial lining thickens to prepare for the potential implantation of a fertilized egg. If implantation doesn’t occur, the endometrium is shed during menstruation.
Endometrial Thickness Normal Size in mm:
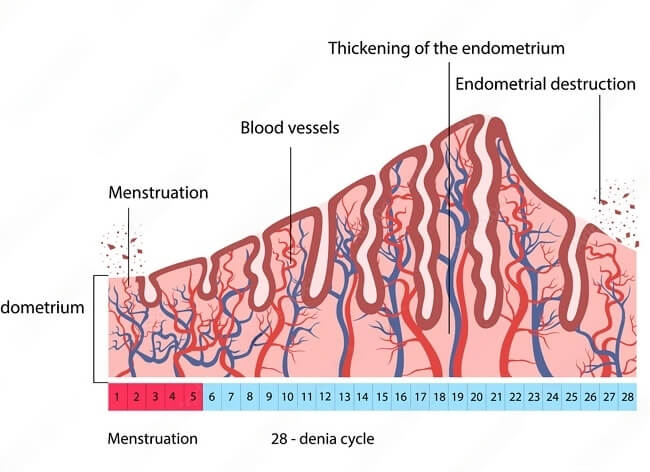
The normal range is approx 2-16 mm, with the endometrium being thinnest during menstruation and thickest during the secretory phase. Here are normal endometrial thickness in different menstrual cycle phases:
- Menstrual phase (days 1-5): 2-4 mm
- Early proliferative phase (days 6-14): 5-7 mm
- Late proliferative phase (days 15-21): 8-11 mm
- Secretory phase (days 22-28): 12-16 mm
Endometrial Thickness Before Period:
The endometrial lining reaches its maximum thickness during the secretory phase (days 22-28) of the menstrual cycle. This phase follows ovulation, and the endometrium is prepared for the possible implantation of a fertilized egg. The endometrial thickness during this phase ranges from 12 to 16 mm.
If implantation does not occur, the endometrium begins to break down, leading to menstruation. Just before the period starts, the endometrial thickness decreases, and it is usually around 2 to 4 mm during menstruation (days 1-5).
Endometrial Thickness During Ovulation:
Ovulation typically occurs around the middle of the menstrual cycle (days 14-16), during the late proliferative phase. The endometrium thickens in response to rising estrogen levels, preparing itself for potential implantation. During ovulation, endometrial thickness is generally between 8 and 11 mm.
Endometrial Thickness in Phases of Menstrual Cycle:
Endometrial Thickness in Phases of Menstrual Cycle
To gain a deeper understanding of endometrial, let’s explore the changes in each phase of the menstrual cycle:
- Menstrual Phase (days 1-5): During menstruation, the endometrial lining is shed, resulting in the period. The endometrial thickness is at its lowest during this phase, ranging from 2 to 4 mm.
- Early Proliferative Phase (days 6-14): Following menstruation, the endometrium begins to regenerate and thicken in response to increased estrogen levels. The endometrial thickness during the early proliferative phase ranges from 5 to 7 mm.
- Late Proliferative Phase (days 15-21): The late proliferative phase encompasses ovulation, during which the endometrium continues to thicken. This phase prepares the uterus for the possible implantation of a fertilized egg. The endometrial thickness during this phase is generally between 8 and 11 mm.
- Secretory Phase (days 22-28): The secretory phase follows ovulation, and the endometrium reaches its maximum thickness in preparation for potential implantation. The endometrial lining becomes more vascular and glandular to support a fertilized egg. The endometrial thickness during the secretory phase ranges from 12 to 16 mm.
If implantation does not occur, the endometrium begins to break down, leading to the next menstrual period and the cycle starts anew.
Endometrial thickness is an essential aspect of a woman’s reproductive health, as it reflects the changes in the uterus lining throughout the menstrual cycle. Before the period, the endometrial thickness decreases, while during ovulation, it ranges between 8 and 11 mm. Understanding endometrial thickness in different phases of the menstrual cycle can provide valuable insights into fertility and overall health. It’s important to remember that individual factors like age, medical history, and fertility goals should be considered when assessing endometrial thickness. Always consult a healthcare professional for personalized advice and guidance.
Also Read: What is Normal Ovary Size
Endometrial Thickness in Pregnancy:
During pregnancy, the endometrial lining—also known as the decidua—undergoes significant changes to support the developing fetus. The decidua consists of three layers: the decidua basalis, the decidua capsularis, and the decidua parietalis.
The decidua basalis is part of the endometrium where the embryo implants, and it later becomes the maternal part of the placenta. The decidua capsularis surrounds the implanted embryo, while the decidua parietalis lines the rest of the uterine cavity.
Throughout pregnancy, the endometrial thickness continues to change, influenced by factors such as hormonal levels, placental development, and fetal growth. It is crucial to maintain an adequate endometrial thickness during pregnancy to ensure proper fetal development and a healthy pregnancy outcome.
Ideal Endometrial Thickness for Pregnancy:
Adequate endometrial thickness is essential for embryo implantation and successful pregnancy. Although there is no universally agreed-upon ideal endometrial , several studies have found a correlation between thicker endometrial linings and higher pregnancy success rates.
The ideal endometrial thickness for pregnancy varies depending on individual factors, but a general guideline is that a of 8 mm or more is considered favorable for embryo implantation. The endometrial lining usually reaches this during the late proliferative phase (days 15-21) of the menstrual cycle.
It is essential to note that while endometrial thickness plays a crucial role in pregnancy success, other factors, such as embryo quality and uterine receptivity, also significantly impact pregnancy outcomes.
Also Read: Ovary Meaning in Hindi
Normal Endometrial Thickness for Pregnancy:
As mentioned earlier, an endometrial of 8 mm or more is generally considered favorable for pregnancy. However, the normal range for endometrial thickness during pregnancy is quite broad, and successful pregnancies have been reported with thinner endometrial linings.
The following are normal endometrial thickness for pregnancy:
- 8-14 mm: This range is typically considered optimal for embryo implantation and successful pregnancy. A thicker endometrium within this range has been associated with higher pregnancy success rates in some studies.
- Less than 8 mm: Although less favorable, successful pregnancies have been reported with endometrial below 8 mm. However, thinner endometrial linings may be associated with lower pregnancy success rates and a higher risk of pregnancy complications, such as miscarriage.
It is important to remember that endometrial thickness is only one-factor influencing pregnancy outcomes. Age, overall health, hormonal balance, and embryo quality also play essential roles in determining pregnancy success.
Endometrial thickness is a vital aspect of a woman’s reproductive health, as it can significantly impact pregnancy outcomes. An endometrial thickness of 8 mm or more is generally considered favorable for pregnancy, but successful pregnancies have been reported with thinner endometrial linings. During pregnancy, the endometrial lining undergoes significant changes to support the developing fetus. It’s crucial to consider individual factors, such as age, overall health, and hormonal balance when assessing endometrial for pregnancy. Consult a healthcare professional for personalized advice and guidance to improve the chances of a successful pregnancy.
Normal Endometrial Thickness in Premenopausal Women:
In premenopausal women, endometrial thickness fluctuates throughout the menstrual cycle, influenced by hormonal changes. Here are general guidelines for endometrial thickness in different phases of the menstrual cycle:
- Menstrual phase (days 1-5): 2-4 mm
- Early proliferative phase (days 6-14): 5-7 mm
- Late proliferative phase (days 15-21): 8-11 mm
- Secretory phase (days 22-28): 12-16 mm
The endometrial lining thickens in preparation for the potential implantation of a fertilized egg and is shed during menstruation if pregnancy does not occur.
Also Read: Uterus Meaning in Hindi
Normal Endometrial Thickness in Postmenopausal Women:
After menopause, estrogen levels decrease significantly, leading to changes in the endometrium. In postmenopausal women, the endometrium typically becomes thinner due to the lack of hormonal stimulation. A normal endometrial for postmenopausal women is 4 mm or less when measured using transvaginal ultrasound.
However, it’s important to consider individual factors and medical history when assessing endometrial thickness in postmenopausal women. In some cases, an endometrial thickness greater than 4 mm can be seen in women on hormone replacement therapy (HRT) or those with specific medical conditions. An unusually thickened endometrium in postmenopausal women may warrant further evaluation, as it can sometimes be a sign of endometrial hyperplasia or other abnormalities.
Is 14 mm Endometrial Thickness Normal?
A 14 mm endometrial thickness falls within the normal range for the secretory phase of the menstrual cycle (days 22-28). It indicates that the endometrium is well-prepared for the potential implantation of a fertilized egg. However, it’s essential to consider other factors like age, medical history, and fertility goals when assessing endometrial .
Also Read: Bulky Uterus In Hindi
Is 1.5 cm (15 mm) Endometrial Thickness Normal?
A 1.5 cm (15 mm) endometrial thickness is also considered normal during the secretory phase of the menstrual cycle. It’s slightly on the higher end of the normal range, but still within acceptable limits for a healthy endometrium. Again, it’s crucial to consider the individual’s context when evaluating endometrial thickness.
In summary, endometrial is a vital aspect of a woman’s reproductive health, with the normal range varying throughout the menstrual cycle. A 14 mm or 1.5 cm endometrial falls within the normal range for the secretory phase, indicating a well-prepared endometrium for potential implantation. However, it’s important to remember that individual factors like age, medical history, and fertility goals should be considered when assessing endometrial thickness. Always consult a healthcare professional for personalized advice and guidance.
Abnormal Endometrial Thickness Treatment:
Abnormal endometrial thickness can be the result of various conditions, such as endometrial hyperplasia, polyps, or endometrial atrophy. Treatment options depend on the underlying cause, individual factors, and the patient’s goals, such as fertility preservation or symptom management. Some common treatment options include:
- Hormonal therapy: Hormone-based treatments, such as progestin therapy or combined estrogen-progestin therapy, can help regulate the endometrial lining and address conditions like endometrial hyperplasia. Hormonal therapies can be administered orally, as injections, or through intrauterine devices (IUDs).
- Hysteroscopy: A hysteroscopy is a minimally invasive procedure that allows doctors to examine the inside of the uterus and remove polyps or other abnormalities.
- Dilation and curettage (D&C): A D&C involves dilating the cervix and using a curette to remove endometrial tissue. This procedure may be recommended for heavy bleeding or to remove abnormal tissue, such as polyps.
- Endometrial ablation: Endometrial ablation is a procedure that destroys the endometrial lining to reduce heavy menstrual bleeding. This treatment is generally not recommended for women who wish to become pregnant in the future.
- Surgery: In some cases, surgery may be necessary to address the underlying cause of abnormal endometrial, such as removing fibroids or treating endometriosis.
It’s essential to consult with a healthcare professional to determine the most appropriate treatment based on individual factors and medical history.
Endometrial Thickness for IVF:
In the context of IVF, endometrial is an important factor that can influence implantation success and pregnancy outcomes. An endometrial thickness of 8-14 mm is generally considered optimal for embryo transfer, with some studies suggesting that a thickness of at least 7 mm is necessary for successful implantation.
If a patient undergoing IVF has a thin endometrium, several interventions may be considered to improve endometrial receptivity, including:
- Estrogen therapy: Oral, transdermal, or vaginal estrogen supplementation can help increase endometrial and improve receptivity.
- Aspirin: Low-dose aspirin therapy may improve blood flow to the uterus and enhance endometrial development.
- Growth factors: In some cases, the administration of growth factors, such as granulocyte colony-stimulating factor (G-CSF), may help improve endometrial.
- Acupuncture: Some studies suggest that acupuncture may improve endometrial receptivity and increase endometrial blood flow.
It’s crucial to work closely with fertility specialists to determine the best approach to optimize endometrial thickness and receptivity for IVF.
Also Read: What is Cyst Meaning in Hindi
When to See a Doctor?
It’s important to consult a healthcare professional if you experience any of the following symptoms, as they may indicate abnormal endometrial thickness or other reproductive health issues:
- Irregular, heavy, or prolonged menstrual bleeding
- Postmenopausal bleeding
- Pain or discomfort during intercourse
- Unexplained pelvic pain
- Difficulty conceiving or recurrent miscarriages
A healthcare professional can help determine the cause of these symptoms, evaluate endometrial , and recommend appropriate treatment options based on individual factors and medical history.
Conclusion:
Abnormal endometrial thickness can result from various conditions and may impact fertility and overall reproductive health. Treatment options for abnormal endometrial depend on the underlying cause and individual factors. In the context of IVF, endometrial thickness is crucial for implantation success, with a thickness of 8-14 mm generally considered optimal. Interventions to improve endometrial receptivity may be necessary for patients with a thin endometrium undergoing IVF.
It’s essential to consult a healthcare professional if you experience symptoms that may indicate abnormal endometrial or other reproductive health issues. Collaborating with healthcare providers can help determine the most appropriate treatment options and optimize reproductive outcomes.
F.A.Q:
Q: Is 7.5 mm endometrial thickness normal?
A: Endometrial varies depending on the menstrual cycle phase and age. In the proliferative phase of the menstrual cycle, an endometrial thickness of around 5-7 mm is normal. In the secretory phase, it can be up to 14 mm. 7.5 mm endometrial thickness may be considered normal depending on the individual’s circumstances.
Q: What happens if the endometrium is thick?
A: Thickening of the endometrium can occur due to several reasons, such as hormonal imbalances, polyps, or cancer. The thickening of the endometrium may cause abnormal uterine bleeding, pelvic pain, or difficulty getting pregnant. In some cases, the thickening of the endometrium may require further investigation and treatment.
Q: When should I worry about endometrial thickness?
A: You should worry about endometrial if it is outside the normal range or if you experience any abnormal symptoms such as abnormal vaginal bleeding, pelvic pain, or difficulty getting pregnant. In these cases, you should consult a healthcare provider for further evaluation and treatment.
Q: What endometrial thickness is abnormal?
A: Endometrial thickness above 14 mm in premenopausal women or 8 mm in postmenopausal women is considered abnormal and may require further investigation.
Q: Can I get pregnant with 7.5 mm endometrium?
A: Yes, it is possible to get pregnant with 7.5 mm endometrial thickness, especially during the proliferative phase of the menstrual cycle when the endometrium is still growing.
Q: Can I get pregnant with 7.7 mm endometrium?
A: Yes, it is possible to get pregnant with 7.7 mm endometrial , especially during the proliferative phase of the menstrual cycle when the endometrium is still growing.
Q: Is 8 mm endometrial thickness normal?
A: Endometrial of 8 mm or less is normal in postmenopausal women. However, in premenopausal women, it may be considered thin for the secretory phase of the menstrual cycle.
Q: What is the treatment for endometrial thickness?
A: The treatment for endometrial depends on the underlying cause. If the cause is hormonal imbalances, hormone therapy may be prescribed. If there are polyps or fibroids, surgical intervention may be required. If the endometrial is due to cancer, treatment may include surgery, chemotherapy, or radiation therapy. It is important to consult your healthcare provider to get a proper diagnosis and treatment.
Q: Is endometrial thickness curable?
A: Endometrial thickness is not a disease or condition on its own, but rather a symptom of an underlying issue. The treatment for endometrial thickness depends on the underlying cause. In many cases, the underlying condition can be treated and the endometrial can resolve.
Q: How much endometrial thickness is good?
A: Endometrial can vary depending on the menstrual cycle phase and age. In the proliferative phase of the menstrual cycle, an endometrial thickness of around 5-7 mm is normal. In the secretory phase, it can be up to 14 mm. However, the optimal thickness for pregnancy is 8-11 mm.
Q: What are the symptoms of endometrial ?
A: Endometrial itself does not typically cause symptoms. However, the underlying condition causing the thickening may cause symptoms such as abnormal vaginal bleeding, pelvic pain, or difficulty getting pregnant.
Q: Can I get pregnant with 8mm endometrium?
A: Yes, it is possible to get pregnant with an 8 mm endometrial , especially during the secretory phase of the menstrual cycle when the endometrium is at its thickest and most receptive to implantation.
Q: Is 7 endometrial thickness normal?
A: Endometrial thickness can vary depending on the menstrual cycle phase and age. In the proliferative phase of the menstrual cycle, an endometrial thickness of around 5-7 mm is normal. However, in the secretory phase, it may be considered thin.
Q: How many mm is a normal endometrial lining?
A: Endometrial thickness can vary depending on the menstrual cycle phase and age. In premenopausal women, a normal endometrial thickness can range from 2-14 mm depending on the phase of the menstrual cycle. In postmenopausal women, a normal endometrial thickness is typically less than 8 mm.


