What is Pelvic Inflammatory Disease (PID)?
Pelvic Inflammatory Disease
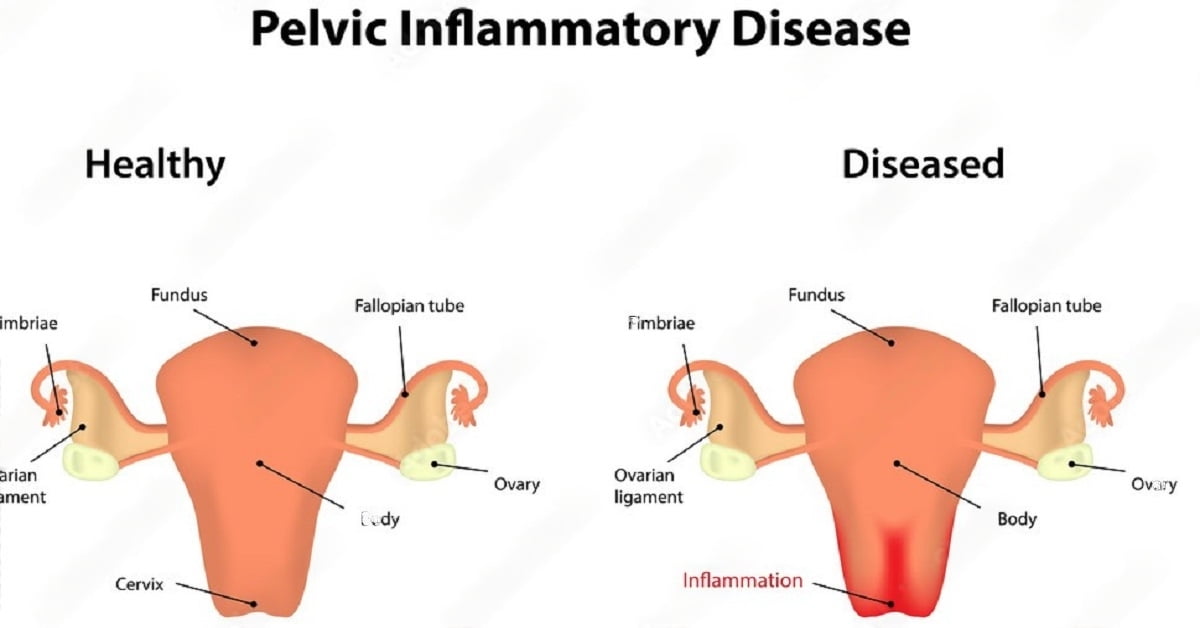
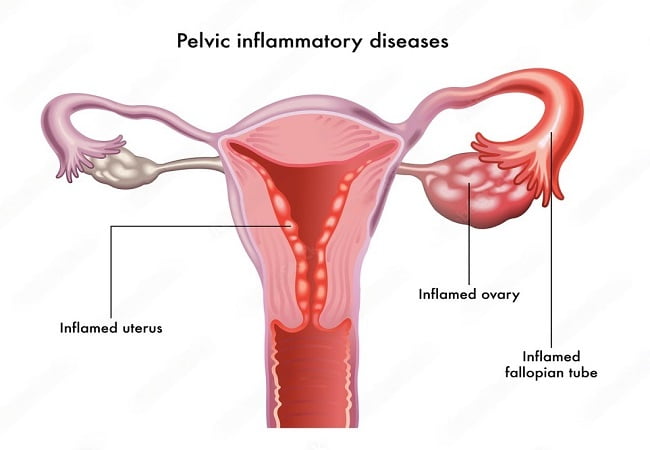
Pelvic Inflammatory Disease (PID) is an infection that occurs in a woman’s reproductive organs. It usually begins with a bacterial infection that spreads from the vagina and cervix to the uterus, fallopian tubes, and ovaries. If left untreated, PID can lead to serious complications, including chronic pain, infertility, and even life-threatening issues like ectopic pregnancies.
The Connection Between PID and Fertility
One of the most significant concerns with PID is its potential impact on fertility. When the infection spreads to the fallopian tubes, it can cause inflammation and scarring, which may block the tubes and prevent eggs from being fertilized. This damage can be irreversible, making it difficult or impossible for some women to conceive naturally.
Does this mean all women with PID will struggle with fertility? Not necessarily, but it does increase the risk. The sooner PID is diagnosed and treated, the less likely it is to cause long-term damage.
Symptoms of Pelvic Inflammatory Disease (PID):
PID can be sneaky, presenting with mild symptoms or none at all. However, it’s essential to recognize the signs and seek medical attention if you suspect you may have the condition. Some common symptoms of PID include:
- Pain: Lower abdominal pain, often described as a dull ache or cramping, is one of the most prevalent symptoms of PID. This pain may worsen during sexual activity or bowel movements.
- Abnormal discharge: A change in vaginal discharge, such as an increase in volume, unusual color, or foul odor, can signal an infection.
- Fever: A fever, often accompanied by chills, can indicate that your body is fighting an infection.
- Irregular menstrual bleeding: PID can cause abnormal bleeding between periods or heavier-than-usual menstrual bleeding.
- Painful urination: Experiencing pain or discomfort while urinating is another sign of PID.
It’s important to remember that these symptoms can also be associated with other conditions. If you experience any of these signs, it’s crucial to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Causes of Pelvic Inflammatory Disease (PID):
Understanding the causes of PID can help us take the necessary steps to prevent it. The primary cause of PID is bacterial infections, with the most common culprits being:
- Sexually transmitted infections (STIs): Chlamydia and gonorrhea are the main known causes of PID. These STIs are easily transmitted through unprotected sexual activity, emphasizing the importance of safe sex practices.
- Other bacterial infections: Although less common, other bacteria can also cause PID. These infections may result from procedures such as intrauterine device (IUD) insertion, childbirth, or abortion, which can introduce bacteria into the reproductive tract.
Prevention of PID:
Prevention is the best medicine when it comes to PID. Some steps you can take to reduce your risk include:
- Practice safe sex: Use condoms consistently and correctly to minimize your exposure to STIs.
- Get tested regularly: If you’re sexually active, get tested for STIs regularly, especially if you have multiple partners or are in a non-monogamous relationship.
- Pay attention to hygiene: Proper hygiene practices, such as wiping front to back after using the toilet, can help prevent the spread of bacteria to your reproductive tract.
- Discuss risks with your healthcare provider: If you’re considering an IUD or planning a pregnancy, talk to your healthcare provider about the potential risks and benefits, as well as any steps you can take to minimize the risk of infection.
If you are diagnosed with PID, it’s crucial to follow your healthcare provider’s recommendations for treatment. This often includes a course of antibiotics to fight the infection. It’s essential to complete the entire prescribed course of medication, even if your symptoms improve, to ensure that the infection is fully eradicated.
In some cases, your partner may also to prevent reinfection. Open communication with your partner about your diagnosis and treatment is crucial for a successful recovery and prevention of future infections.
For more severe cases of PID, hospitalization and intravenous antibiotics may be necessary. In rare instances, surgery might be required to remove abscesses or repair damage caused by the infection.
Complications of Pelvic Inflammatory Disease (PID):
PID can lead to various complications if left untreated. These complications can have a lasting impact on a woman’s health and well-being. Some of the most common complications include:
- Chronic pelvic pain: PID can cause long-term pelvic pain that may persist even after treatment. This pain can negatively affect a woman’s quality of life and make daily activities challenging.
- Infertility: As mentioned in our previous article, PID can lead to infertility by causing scarring and blockage in the fallopian tubes. This damage can make it difficult or impossible for some women to conceive naturally.
- Ectopic pregnancy: PID increases the risk of ectopic pregnancies, which occur when a fertilized egg implants outside the uterus, often in a fallopian tube. This condition is life-threatening and requires immediate medical attention.
- Abscess formation: PID can cause abscesses, which are collections of pus that develop as a result of infection. These may require surgical intervention if antibiotics aren’t effective.
Diagnosing Pelvic Inflammatory Disease (PID):
Diagnosing PID can be a challenge, as the symptoms can be vague and mimic other conditions. However, early diagnosis is crucial to prevent long-term complications. Some common methods of diagnosing PID include:
- Medical history and physical examination: Your healthcare provider will begin by asking about your symptoms, sexual history, and menstrual cycle. They will also perform a physical examination, checking for signs of PID, such as tenderness in the pelvic area.
- Laboratory tests: Lab tests, such as a blood test or a cervical swab, can help identify the bacteria causing the infection. Your healthcare provider may also test for sexually transmitted infections (STIs) like chlamydia and gonorrhea.
- Imaging studies: In some cases, imaging studies like ultrasounds or CT scans may be necessary to assess the extent of the infection and check for complications, such as abscesses or damage to the reproductive organs.
Treatment for Pelvic Inflammatory Disease (PID):
- Antibiotic therapy: The primary treatment for PID is antibiotic therapy. Your healthcare provider will prescribe a course of antibiotics to target the specific bacteria causing the infection. It’s essential to take the medication as prescribed and complete the entire course, even if your symptoms improve.
- Pain management: Your healthcare provider may recommend over-the-counter pain relievers, such as ibuprofen or naproxen, to help manage pain and inflammation.
- Hospitalization: In severe cases or when complications are present, hospitalization may be necessary. This allows for intravenous antibiotic administration and close monitoring of your condition.
- Surgery: In rare cases, surgery may be required to treat complications, such as abscesses or severe damage to the reproductive organs. Surgical intervention might include draining abscesses or, in extreme cases, removing damaged tissue or organs.
- Partner treatment: If PID is caused by an STI, your partner may also need treatment to prevent reinfection. Open communication and mutual support can be crucial in overcoming this challenging experience together.
Risk Factors for Pelvic Inflammatory Disease:
Understanding the risk factors for PID can help you make informed decisions about your health. Some common risk factors include:
- Sexually transmitted infections (STIs): Chlamydia and gonorrhea are the leading causes of PID, making those with these STIs more susceptible to the disease.
- Multiple sexual partners: Having multiple partners increases the risk of contracting an STI, subsequently raising the risk of developing PID.
- Age: Younger women, particularly those under 25, are at a higher risk for PID due to their increased likelihood of contracting STIs.
- History of PID: If you’ve had PID before, you’re at a greater risk of developing it again.
- Intrauterine device (IUD) insertion: The risk of PID can be slightly increased in the first few weeks after IUD insertion.
Lowering Your Risk for PID:
Although it may not be possible to eliminate the risk of PID entirely, there are steps you can take to reduce your chances of developing the condition:
- Practice safe sex: Consistently using condoms can significantly reduce the risk of contracting STIs, which are the primary cause of PID.
- Get regular STI testing: Early detection and treatment of STIs can help prevent the development of PID.
- Limit your number of sexual partners: Reducing the number of sexual partners decreases the likelihood of contracting an STI and, subsequently, PID.
- Consider your contraceptive choices: Talk to your healthcare provider about the best contraceptive options for you, taking into account your risk for PID.
Preventing Pelvic Inflammatory Disease:
Prevention is the key when it comes to PID. While you cannot guarantee that you’ll never develop the condition, following the steps mentioned above can significantly lower your risk. Maintaining open communication with your healthcare provider and partner(s) about your sexual health can also contribute to prevention.
Is There a Permanent Cure for Pelvic Inflammatory Disease?
PID can be treated effectively with antibiotics, and in most cases, women can make a full recovery. However, it’s important to note that antibiotic treatment may not reverse any damage already done to the reproductive organs. This is why early detection and treatment are crucial.
How to Test Yourself for PID?
Unfortunately, there is no at-home test for PID. However, if you suspect you might have PID, it’s essential to see your healthcare provider as soon as possible. They will perform a physical examination, take a medical history, and may order lab tests or imaging studies to make an accurate diagnosis.
If you’re concerned about your risk for STIs, there are at-home testing options available. These tests can help detect infections like chlamydia and gonorrhea, which, if left untreated, can lead to PID. However, it’s essential to follow up with a healthcare provider for a comprehensive evaluation and appropriate treatment.
Does Pelvic Inflammatory Disease Show on Ultrasound?
While ultrasounds can’t diagnose PID directly, they can help detect some of the complications associated with the condition. Ultrasounds may reveal abnormalities, such as fluid collection, abscesses, or inflammation in the pelvic organs. However, it’s essential to remember that ultrasounds are just one diagnostic tool, and healthcare providers rely on a combination of methods, including medical history, physical examination, and laboratory tests, to accurately diagnose PID.
What Antibiotics Treat Pelvic Inflammatory Disease?
Antibiotics are usually the first line of treatment for PID. The choice of antibiotics depends on the specific bacteria causing the infection. Typically, healthcare providers prescribe a combination of antibiotics to ensure effective treatment against a wide range of bacteria. Some commonly used antibiotics for PID include:
- Ceftriaxone
- Doxycycline
- Metronidazole
It’s crucial to follow your healthcare provider’s instructions and complete the entire course of antibiotics, even if your symptoms improve, to ensure the infection is fully treated.
Can Amoxicillin Treat Pelvic Inflammatory Disease?
Amoxicillin is an antibiotic that belongs to the penicillin family. While it’s effective against certain bacterial infections, it’s not typically recommended as a first-line treatment for PID. This is because PID-causing bacteria, like chlamydia and gonorrhea, often respond better to other antibiotics, such as those mentioned above. However, your healthcare provider may consider using amoxicillin in specific cases, depending on the bacteria involved and your individual circumstances.
PID Without STD:
Although sexually transmitted infections (STIs) like chlamydia and gonorrhea are the leading causes of PID, it’s possible to develop the condition without having an STI. Non-sexually transmitted causes of PID include:
- Bacterial infections following childbirth, miscarriage, or abortion
- Use of an intrauterine device (IUD), particularly during the first few weeks after insertion
- Invasive gynecological procedures, such as dilation and curettage (D&C) or endometrial biopsy
It’s essential to discuss your risk factors and any concerns with your healthcare provider to ensure appropriate diagnosis and treatment.
Fertility Concerns: Will I Have Trouble Getting Pregnant If I Had PID?
PID can potentially impact your fertility, depending on the severity of the infection and any damage caused to your reproductive organs. If PID leads to scarring or blockages in the fallopian tubes, it can make it difficult for an egg to travel to the uterus, resulting in fertility issues.
However, not all women who have had PID will face fertility problems. Early detection and prompt treatment can significantly reduce the risk of long-term complications, including infertility. If you’re concerned about your fertility after having PID, it’s essential to discuss your concerns with your healthcare provider. They can provide guidance and, if necessary, refer you to a fertility specialist for further evaluation and support.
Navigating the Emotional Challenges of PID
Dealing with PID can be emotionally challenging, especially when considering potential impacts on fertility and the complexity of diagnosis and treatment. It’s essential to remember that you’re not alone on this journey. Reach out to friends, family, or support groups for emotional encouragement and guidance. By educating yourself and taking proactive steps, you can regain some
Conclusion
Understanding the various aspects of Pelvic Inflammatory Disease (PID), such as detection through ultrasound, appropriate treatment options, the possibility of non-STD-related PID, and the impact on fertility, is essential for those affected by this condition. Early diagnosis, effective treatment, and open communication with healthcare providers are crucial for managing PID and mitigating potential complications. By staying informed, taking proactive measures, and seeking support from loved ones, individuals dealing with PID can navigate their journey toward better health and well-being with confidence and resilience.
F.A.Q
Q: What are the 6 symptoms of PID?
A: Six common symptoms of pelvic inflammatory disease (PID) include lower abdominal pain, fever, vaginal discharge, painful intercourse, irregular menstrual bleeding, and painful urination.
Q: What is the main cause of pelvic inflammatory disease?
A: The main cause of PID is a bacterial infection that usually starts in the cervix and spreads to the upper reproductive organs, including the uterus, fallopian tubes, and ovaries. The most common bacteria responsible for PID are Chlamydia trachomatis and Neisseria gonorrhoeae, which are typically transmitted through sexual contact.
Q: What are the 3 symptoms of PID?
A: Three common symptoms of pelvic inflammatory disease (PID) are abdominal pain, vaginal discharge, and painful intercourse.
Q: Is pelvic inflammatory disease serious?
A: Yes, PID can be a serious condition if left untreated. It can cause permanent damage to the reproductive organs, leading to infertility, chronic pelvic pain, and ectopic pregnancy. In severe cases, PID can also lead to sepsis and death.
Q: How do you confirm PID?
A: PID can be confirmed through a combination of medical history, physical examination, and laboratory tests. Tests may include a pelvic exam, ultrasound, blood tests, and cultures of vaginal and cervical discharge.
Q: What is the 4 stage of PID?
A: There is no specific “fourth stage” of PID. However, PID can progress through several stages, starting with infection of the cervix and spreading to the uterus, fallopian tubes, and ovaries. In severe cases, PID can lead to abscess formation and sepsis.
Q: What is the best treatment for PID?
A: Treatment for PID typically involves antibiotics to kill the bacteria causing the infection. In some cases, hospitalization may be necessary for intravenous antibiotics and monitoring. Treatment may also involve pain management, rest, and avoiding sexual activity until the infection has cleared.
Q: What is the fastest way to cure PID?
A: There is no fast way to cure PID, as treatment typically involves a course of antibiotics that can take several weeks to fully clear the infection. It’s important to start treatment as soon as possible to avoid complications and permanent damage to the reproductive organs.
Q: Can pelvic inflammatory disease be cured?
A: Yes, pelvic inflammatory disease (PID) can be cured with appropriate treatment, which typically involves antibiotics. However, prompt diagnosis and treatment are important to prevent complications and permanent damage to the reproductive organs.
Q: What is the early stage of PID?
A: The early stage of PID typically involves infection of the cervix and spreading of the bacteria to the uterus and fallopian tubes. This can cause mild symptoms or no symptoms at all, making early detection and treatment difficult.
Q: What age is PID common?
A: PID can occur at any age after a woman becomes sexually active, but it is most common among young women between the ages of 15 and 24.
Q: What organ is affected by PID?
A: Pelvic inflammatory disease (PID) is known to affect the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It is typically caused by a bacterial infection that spreads from the cervix.
Q: Can PID be cancerous?
A: No, PID itself is not cancerous. However, untreated or recurrent PID can lead to complications that increase the risk of developing certain types of cancer, such as ovarian cancer.
Q: What antibiotics treat PID?
A: Antibiotics that are effective against the bacteria causing PID, such as doxycycline and ceftriaxone, are typically used to treat the infection. In some cases, a combination of antibiotics may be prescribed.
Q: Can I get pregnant with PID?
A: PID can affect fertility and increase the risk of ectopic pregnancy, but it does not always cause infertility. Early diagnosis and treatment can reduce the risk of complications and improve the chances of getting pregnant.
Q: What is the early stage of PID?
A: The early stage of PID typically involves infection of the cervix and spreading of the bacteria to the uterus and fallopian tubes. This can cause mild symptoms or no symptoms at all, making early detection and treatment difficult.